Should the NHS really use magic mushrooms to treat mental health?


Pallab GhoshScience Correspondent
 BBC
BBCListen to Pallab Ghosh read this article
Larissa Hope truly believes that psilocybin, the active ingredient in magic mushrooms, saved her life.
Back when she was 17 and starting out as an actress, she was cast in the TV drama Skins, but the new-found fame brought out a previously buried trauma. She didn’t find antidepressants effective – but that small dose of psilocybin, which she took under clinical supervision, marked a turning point.
“When I experienced it, I burst out crying,” she says today. “It was the first time in my life I had ever felt a sense of belonging and safety in my body I kept saying, ‘I’m home, I’m home’.”
Now, almost 20 years on, Larissa maintains that it was this, along with therapy, helped her confront suicidal feelings.
Not everyone feels the same. Jules Evans, a university researcher, had a very different experience when he first took LSD, albeit for recreational purposes, back when he was 18.
The trip sent him into what he describes as a “deluded” state.
 Jules Evans
Jules Evans“I believed that everyone was talking about me, criticising me, judging me. I thought, I’ve permanently damaged myself; I’ve permanently lost my mind.
“It was the most terrifying experience of my life.”
Today he is director of the Challenging Psychedelic Experiences Project, which helps people experiencing difficulties after taking psychedelics. He says he felt socially anxious and suffered from panic attacks years after his own experience and was diagnosed with post-traumatic stress disorder (PTSD).
But these two starkly different experiences are at the heart of a dilemma currently facing doctors, regulators and politicians.
That is: should doctors be allowed to prescribe treatments that involve the use of magic mushrooms and other potentially useful psychedelic drugs?
Magic mushrooms and depression
The question has come to the fore amid a series of new studies that suggest psychedelic drugs could help treat depression, obsessive-compulsive disorder, PTSD, trauma and addictions such as alcohol and gambling.
The use of psychedelic medicine is illegal at present unless in authorised research or clinical trials. But since 2022, more than 20 such trials have tested different psychedelic medicines for conditions such as depression, PTSD, and addiction.
The results of many of these studies suggest that the treatments can help, while several others have mixed or unclear results.
Only a few so far have clearly found no benefit on their main measures.
Results from one of the largest clinical trials into the use of psilocybin, by UK biotech firm Compass Pathways, is due later this year.
The UK’s medicines regulator is waiting for this data as it considers whether to relax the current tight restrictions and allow use of the psychedelic medicine outside research and trials.
Prof Oliver Howes, chair of the Royal College of Psychiatrists’ Psychopharmacology Committee, is optimistic. He says he sees psychedelics as a promising potential new treatment for psychiatric disorders – including for patients in the NHS.
“One of the key messages is that this is something we desperately need – more treatments and better treatments for mental health disorders…
“These treatments are really interesting because they’ve shown promise in these small-scale studies… and have the potential to work quicker.”
But he is also cautious, emphasising the need to see results from the trials. “It’s really important that we get evidence and not overhype the potential benefits.”
Others have also urged caution. A report by the Royal College of Psychiatrists, published in September 2025, warned of the potential dangers of psychedelics, and doctors also stress that taking psychedelic drugs is not just illegal but can also be harmful.
Faster acting, fewer side effects?
Drug use is as old as civilisation itself. Magic mushrooms, opium and cannabis have long been used for both recreation and rituals.
By the 1960s and 1970s, LSD, also known as acid, was used by the counterculture movement, with Harvard psychologist and counterculture guru, Timothy Leary, urging young people to “turn on, tune in, drop out”. In other words, to turn on and awaken their inner potential, tune in to the state of society around them and to drop out of social norms of the time.
But soon, these drugs were associated with social unrest and moral decline.
 Getty Images
Getty ImagesBy the time they were banned in the late 1960s and early 1970s, greater restrictions were being applied to scientific research around them too.
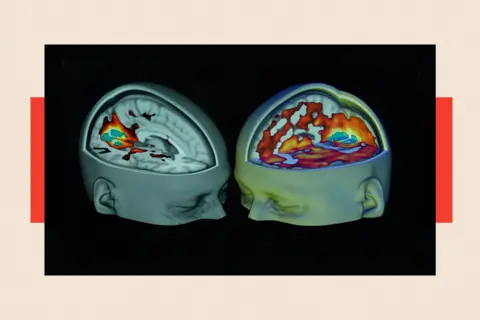
But a series of ground-breaking scientific developments in the 2010s by Prof David Nutt and his team at Imperial College London began a process that may well end up changing that.
Subsequent clinical trials on depressed patients indicated that psilocybin was at least as effective as conventional anti-depressants, and with fewer side effects. But there was another big advantage, according to Prof Nutt: how fast-acting it is.
“We thought rather than wait for eight weeks for antidepressants to switch off the part of the brain associated with depression, maybe psilocybin could switch it off in the space of a few minutes.”
This view, although scientifically promising, is not universally accepted.

Prof Nutt is a respected scientist, but his assertions have generated controversy.
He was dismissed in 2009 as chair of the government’s drugs advisory body, the Advisory Committee on the Misuse of Drugs, by the then Labour Home Secretary Alan Johnson, following certain public comments – such as claiming there was “not much difference” between the harm caused by horse-riding and ecstasy – which were seen as incompatible with his role as a government adviser.
In recent years, Prof Nutt’s studies sparked many more investigations across the world on the potential therapeutic benefits of other psychedelic drugs.
Should they really be available on the NHS?
At University College London, neuroscientist Dr Ravi Das has been trying to understand why some habits harden into addictions while others fade away. He believes psychedelics may help find the answer.
The study he leads has been recruiting heavy drinkers to test whether dimethyltryptamine (DMT), a short-acting psychedelic also used as a recreational drug, can be used to to target the brain’s memory and learning systems.
It builds on evidence suggesting psilocybin can disrupt habitual behaviours linked to addiction.
“Every time someone drinks, a bit like Pavlov’s dog, you’re learning to associate things in the environment with the rewarding effect of alcohol,” he says. “We’ve been focusing on whether certain drugs, such as psychedelics can break down those associations.”
This is a very early-stage study, but if this and future trials are successful, the aim is to offer it as a treatment within the NHS (with regulatory approval).
“If psychedelic therapies prove to be both safe and more effective than current treatments, I would hope to see them made accessible via the NHS — rather than to just the privileged few who can afford them privately,” he says.
Ketamine, which was the subject of a previous trial by Dr Das, sits in a different legal category and can be used as part of a medical treatment in the UK.
Other psychedelics, such as DMT, LSD, psilocybin and MDMA are currently deemed to have no legitimate medical use and so can only be used for research – and even then under very strict and hard-to-obtain medical licenses.
Dr Das believes positive results from trials might change views as the emerging scientific evidence mounts. “I hope if there’s sufficient evidence, the government will be open to revising the scheduling of these drugs,” he says.
However, an analysis, published in the British Medical Journal in November 2024 by a PhD student Cédric Lemarchand and colleagues, questioned how easy it was to determine the precise effect of psychedelic drugs.
“Because hallucinogens are often combined with a psychotherapy component, it is difficult to separate the effects of the drug from the therapeutic context, complicating comprehensive evaluations and product labelling.”
It also suggested short-term trials may not detect “the potential for harm and serious adverse events from long-term use of hallucinogens… The potential for abuse or misuse must also be considered.”
‘People are suffering… It’s a moral failing’
While research suggests therapeutic benefits from psychedelic medicines, doctors remain cautious. Prof Howes believes that – except for ketamine, which has been assessed by the regulator – psychedelic treatments should not be routine medical practice in the UK outside research settings, until larger, more rigorous trials provide more robust evidence for their safety and effectiveness.
“In a clinical trial setting, it’s very carefully evaluated. If people take these on their own or in a backstreet clinic, then there is no guarantee of that and the safety issues start becoming a major issue.”
His warnings are supported by figures from various studies, gathered by Challenging Psychedelic Experiences. It suggests that 52% of respondents who regularly use psychedelic drugs say they have had an intensely challenging psychedelic trip, 39% of whom considered it “one of the five most difficult experiences of their life”.
In addition, 6.7% said they considered harming themselves or others following a challenging experience, and 8.9% reported they were “impaired” for more than a day after a difficult trip.
Some people required medical or psychiatric assistance and continued to feel worse for weeks, months, or in some cases years after their experience, according to Mr Evans.
“Ideally, I would love doctors and regulators to know more about these adverse effects, and how people can recover from them, before they say, any of these therapies are safe,” he argues.
 Compass Pathways
Compass PathwaysBut Prof Nutt, Prof Howes and Dr Das, believe that progress into the clinic is being slowed by the difficulty of obtaining permission to carry out medically supervised clinical trials.
“There are so many people suffering unnecessarily,” Prof Nutt told BBC News. “And some of them are dying, because of the unreasonable barriers to research and treatment that we face in this country. It is, in my view, a moral failing.
“When these medicines are proven to be safe and effective, I think it is vital they are made available through the NHS to all who need them, not limited to the private sector, as happened with medical cannabis.”
Although he urges caution, it is a view shared by Prof Howes.
“There are big barriers to doing this research, so we do ask for the government to review the regulations of these substances, for research, because it does lead to long delays, and, we desperately do need new treatments.”
The analysis from Mr Lemarchand calls for greater scrutiny of trials. “To guarantee that hallucinogens are rigorously vetted before endorsing them as safe and effective treatments medical journals must appraise the evidence more critically, fully account for limitations, avoid spin and unsubstantiated claims, and correct the record when needed.”
The Advisory Council on the Misuse of Drugs is also blunt in stating that Schedule 1 “contains those of no medicinal value,” so they should sit under the tightest controls, it says. Ministers also tie the Home Office licensing regime directly to public protection.

The government has backed plans to ease licensing requirements for some clinical trials approved by the Medicines and Healthcare products Regulatory Agency and Health Research Authority, with work under way to implement exemptions for certain universities and NHS sites. A cross-government working group is co-ordinating the cautious rollout, pending the results of pilot projects.
But some doctors, including Prof Howes, say changes are moving painfully slowly. “There’s still a lot of red tape holding things up,” he says.
Supporters of psychedelic medicines hope that so-called phase three trials by Compass Pathways, will lead to further relaxations, at least on research.
Larissa Hope’s concern is for people in the position she once was in. “It is a reflection of society that psychedelic medicine is not more accessible as a treatment for everyone.
“It could stop so many premature deaths, as it did for me.”
Top Image Credit: Getty Images

BBC InDepth is the home on the website and app for the best analysis, with fresh perspectives that challenge assumptions and deep reporting on the biggest issues of the day. You can now sign up for notifications that will alert you whenever an InDepth story is published – click here to find out how.
Source link


